Artificial Intelligence (AI) and Machine Learning (ML) are changing how doctors read MRI and CT scans. These tools help find health problems faster and more accurately. In hospitals and clinics, radiology machine learning is now part of daily work. It supports radiologists by making diagnostic imaging clear and easy to read.
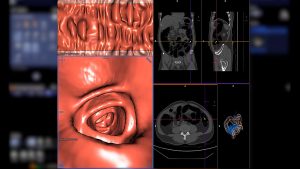
With AI in radiology, we can use machine learning in medical imaging, deep learning MRI analysis, CT image segmentation with AI, and more. These tools help make sense of the huge image sets from MRI and CT. They can assist in automated diagnosis of MRI, CT, image‑based biomarkers, and image reconstruction using AI. For example, a model might find a tumor in a brain MRI or detect lung nodules in a CT faster than before.
In this article, you will learn how AI and ML are changing MRI and CT workflows. We will explore what they are, how they work, and why they matter. We will look at real‑life use cases like brain tumour segmentation AI‑MRI, lung CT AI screening, stroke detection with CT AI, and many more. We will also cover the good things and the problems, such as bias in AI medical imaging, explainable AI in medical imaging, and integration with PACS systems and AI imaging. At the end, we will glimpse into the future: federated learning MRI datasets, edge computing in imaging AI, global health and underserved areas, and more.
Let’s dive into how AI is helping diagnosis in MRI and CT—where big image sets meet smart algorithms—and how that might help doctors, patients, and the health system.
1. Background: Key Concepts & Modalities
1.1 What are MRI and CT?
Magnetic Resonance Imaging (MRI) and Computed Tomography (CT) are two major imaging tools in medicine.
- MRI uses strong magnets and radio waves to create detailed pictures of soft tissues like the brain, muscles, and organs.
- CT uses X‑rays and a rotating scanner to make many cross-sectional images (“slices”) of the body.
- CT gives fast images and is good for bones, lungs, and bleeding. MRI is slower but gives better detail for soft tissues.
12 What is Artificial Intelligence (AI), Machine Learning (ML), and Deep Learning (DL)?
- Artificial Intelligence (AI) means computers doing tasks that normally need human thinking.
- Machine Learning (ML) is a subset of AI where computers learn from data to make predictions or decisions.
- Deep Learning (DL) is a form of ML that uses many layers in a neural network (like a brain model) to learn complex patterns.
These technologies work well with medical imaging because MRI and CT produce lots of complex image data.
1.3 Why MRI/CT + AI is Attractive
- MRI and CT scans create huge amounts of image data every day in clinics worldwide. That data is a good match for ML and DL because machines are good at handling lots of image information.
- AI in radiology can help with image reconstruction using AI and image‑based biomarkers because it can detect tiny patterns in images.
- With MRI and CT, there is a chance to improve accuracy, reduce scan times, and improve workflow with machine learning in medical imaging, automated diagnosis of MRI and CT, and workflow optimisation in radiology using AI.
- Given that radiologists face many scans, AI gives tools like triage of medical images using ML, segmentation‑classification pipeline MRI ML, and using deep neural networks for imaging to assist in finding disease early.
2. How Machine Learning Aids MRI & CT: Applications & Use‑Cases
2.1 Image Acquisition & Reconstruction
AI helps make the scanning process with MRI and CT better and faster. For example:
- In CT scans, AI can reduce radiation dose and improve image clarity.
- In MRI, AI‑based techniques allow faster scans with less motion artefact and still maintain image quality.
- Because large data sets exist for MRI and CT, this suits machine learning in medical imaging, deep neural networks for imaging, and image reconstruction using AI well.
For example, by using convolutional neural networks (CNNs) and deep learning (DL), algorithms can reconstruct full images from fewer or lower‑quality inputs.
2.2 Image Analysis: Segmentation, Detection, Classification
After the scan is done, ML helps in interpreting it. Some tasks:
- Organ/tumour segmentation: AI models delineate boundaries of a tumour in MRI or CT.
- Lesion detection: For example, spotting lung nodules on a CT, or a brain tumour on MRI.
- Classification: Determining whether a lesion is benign or malignant, or grading its severity.
Studies show that in many cases, AI tools are at least matching human radiologists in specific tasks, especially when using large datasets and DL models.
2.3 Workflow Optimisation & Radiologist Assistance
ML doesn’t just help with image pixels; it also helps the radiology workflow:
- Triage of medical images using ML: Urgent scans get flagged so radiologists can prioritise.
- Automated segmentation of organs, automated report generation, and workflow optimisation help speed up work and reduce fatigue.
- The combination of AI + radiologist (human‑machine collaboration in diagnostics) is proving more effective than either alone.
2.4 Multimodal & Predictive Analytics
Beyond MRI or CT alone:
- Combining MRI, CT, and other clinical data (multi-modal imaging machine learning) provides richer information for diagnosis and treatment planning.
- Using AI for predictive modelling from CT scans, risk stratification using MRI, and outcome prediction from CT/MRI helps move toward personalised medicine.
- Techniques such as transfer learning, federated learning, and privacy-preserving AI imaging support training models across multiple centers without sharing raw data.
3. Benefits & Value Proposition

When we use Artificial Intelligence (AI) and Machine Learning (ML) in Magnetic Resonance Imaging (MRI) and Computed Tomography (CT), many benefits arise. Here are the key value points in simple terms:
Improved Diagnostic Accuracy
AI tools help radiologists spot things that are easy to miss by eye. They support image‑based biomarkers using AI, automated diagnosis, and detection of subtle disease signs. Research shows these tools improve accuracy and reduce missed findings.
Faster Scan Times & Better Patient Experience
With AI, MRI and CT procedures can be faster. That means less time in the scanner, less discomfort, and higher throughput. For example, AI helps with image reconstruction using AI and MRI motion artefact reduction, making scans quicker and clearer.
Reduced Radiation Dose & Safer Imaging
For CT scans, especially, AI helps reduce radiation exposure while keeping image quality high. It supports safer workflows and improved patient safety.
Workflow Optimisation & Radiologist Support
AI helps radiology departments run smoothly. It supports triage of medical images using ML, workflow optimisation, and automated segmentation of organs. By doing routine or repetitive tasks, AI frees radiologists to focus on harder cases.
Personalised & Predictive Care
By combining imaging data from MRI and CT with other clinical information, AI models can support predictive modelling from CT scans, risk stratification from MRI AI, and personalised medicine via imaging AI. This can lead to tailored treatment plans for patients.
Better Access & Cost‑Effectiveness
In some settings, AI helps make high‑quality imaging available more broadly and at lower cost. Faster scans, efficient workflows, and fewer repeat exams all contribute to cost savings.
4. Challenges, Risks & Limitations
When we talk about using Artificial Intelligence (AI), Machine Learning (ML), and Deep Learning (DL) in Magnetic Resonance Imaging (MRI) and Computed Tomography (CT), there are many challenges. Here are the key problems to know in simple words.
Data Quality, Bias & Generalisability
- AI models need large, good‐quality labelled datasets. But data may be incomplete, noisy, or biased.
- If the training data comes mostly from one patient group or one type of scanner, the model may not work well for other groups or other machines. This is a generalisability problem.
- There is also the risk of bias in AI medical imaging, where models might favour or perform better for certain populations.
Explainability & Trust
- Many AI and deep learning models work like “black boxes” — they give output (for example: “there is a tumour”), but it is hard to see how they made that decision. That is the explainable AI in medical imaging challenge.
- If doctors cannot trust what the AI is doing or understand it, they may hesitate to use it. That affects human‑machine collaboration in diagnostics.
Regulatory, Workflow & Integration Hurdles
- Bringing an AI system into clinical practice means meeting regulatory rules (for example, approval from authorities). That takes time and effort.
- Integration with existing radiology systems like PACS, DICOM workflows, and clinical decision support is not trivial. The change management and training of staff matter.
- It’s not enough to have a model that works in lab tests — you need it to work in the real world with real hospital workflows.
Artefacts, Scan Variability & Technical Limitations
- Different scanners, settings, patient motion, and artefacts (like movement in MRI) can make image quality vary a lot. An AI model trained on perfect data may struggle with real‑life data.
- For example, a model may do well in “training MRI acquisition & reconstruction” tasks in the lab, but may face image registration AI in multimodal imaging or dataset annotation scarcity in MRI ML in practice.
Ethical, Privacy & Liability Concerns
- Privacy: using large imaging datasets means ensuring patient data is secure and anonymised. That is a privacy‑preserving AI imaging concern.
- Liability: If an AI model makes a wrong diagnosis (e.g., missing a tumour on CT), who is responsible? The doctor, the hospital, the AI vendor? This risk affects adoption.
- Over‑reliance risk: If clinicians depend too much on AI, they may lose skill or fail to check the output carefully.
How to Address These Challenges (Short List)
- Use large, diverse datasets across different scanners, populations, and locations.
- Ensure transparent, interpretable modelling (explainable AI) so users can understand the “why”.
- Rigorous clinical validation, real‑world testing, and continuous monitoring of model performance.
- Staff training, workflow redesign, and IT infrastructure investment for integration.
- Strong governance: privacy, ethics, auditability, and liability frameworks.
- Ongoing maintenance: models drift over time, so they must be updated and monitored for dataset heterogeneity in imaging AI.
5. Future Directions & Trends

Here’s what lies ahead for Artificial Intelligence (AI) in MRI and CT:
Emerging Trends
- AI models will move beyond just analysing images. They will work through the full imaging pipeline: from image acquisition & reconstruction through segmentation, classification, and onto outcome prediction.
- The use of generative adversarial networks (GANs), diffusion models, and other generative AI techniques will allow high‑quality images from less data, for example, faster MRI scans or lower-dose CT scans.
- Multimodal imaging machine learning will grow: combining MRI + CT + clinical data (labs, genomics) to build deeper models for predictive modelling from CT scans and risk stratification MRI AI.
- Federated learning MRI datasets, privacy‑preserving AI imaging, and edge computing in imaging AI will allow models to train across hospitals without sharing raw patient data, improving scale and protecting privacy.
- AI will increasingly adopt transformer architectures, self‑supervised learning, and end‑to‑end modelling for the full workflow, e.g., segmentation‑classification pipeline being embedded inside the scanner acquisition.
Why These Matter
- These advances promise better personalised medicine via imaging AI: decisions tailored to individual patients based on high‑quality image + model analysis.
- They support making scans faster and safer: e.g., MRI motion artefact reduction AI, CT image reconstruction deep learning, fewer contrast agents, less radiation.
- They improve the potential for global health and underserved areas: portable MRI/CT + AI assist where radiology expertise is limited.
Remaining Challenges & How the Future Might Address Them
- Model generalisability across diverse patient cohorts and scanner types remains a hurdle. Future work will require large, diverse datasets and external validation.
- Explainability: Clinicians need to trust AI outputs. Future systems will embed explainable AI (XAI) frameworks for interpretability in imaging AI.
- Workflow integration: Future trends point toward seamless integration of AI into PACS systems, real‑time imaging, and interventional settings — not just as a separate tool.
- Governance, ethics and regulation: As AI becomes more embedded in diagnostics, standards for regulatory approval for AI in radiology, ethical issues AI in diagnostic imaging, and governance of imaging AI will take centre stage.
- Data and annotation bottlenecks: More synthetic data (via generative AI) and automated annotation tools will help address dataset annotation scarcity in MRI ML. For example, generative models may create realistic training scans.
What This Means for You (Clinicians, Radiology Departments, Researchers)
- Start preparing now: adopt tools that support workflow optimisation in radiology AI, but also plan for future integration of end‑to‑end AI pipelines.
- Invest in interoperable systems: ensure your imaging systems support DICOM, PACS, AI plugins, and edge/cloud workflows so you can adopt future AI image workflow integration.
- Engage in data strategy: building or participating in multi‑site data sharing or federated learning frameworks will be key to staying ahead.
- Focus on patient‑centric outcomes: future AI isn’t just about faster or cheaper scans — it’s about improved detection (lesion detection MRI with AI, lung CT AI screening), better stratification, fewer repeat exams, and better outcomes.
- Stay informed about standards and validation: as new AI tools appear, check for evidence of clinical validation, real‑world deployment, and oversight of bias in AI medical imaging and model drift.
6. Practical Guidance for Radiology Departments / Clinicians
Here’s a practical, step‑by‑step guide to help radiology teams adopt Artificial Intelligence (AI) and Machine Learning (ML) in MRI and CT.
6.1 What to look for when evaluating an imaging AI tool
- Ensure the tool is relevant to your clinical goals — e.g., lung CT AI screening, brain tumour segmentation AI‑MRI, automated diagnosis MRI CT.
- Check if the model has external validation, good performance metrics (sensitivity, specificity, AUC). Research shows many tools still lack strong external testing.
- Confirm the tool handles diverse scanners, patient populations, and works with your institution’s imaging protocols (scanner vendors, MRI/CT settings). Avoid dataset heterogeneity in imaging AI problems.
- Review integration needs: Does it connect with your PACS, DICOM workflows, and reporting system? Look for AI image workflow integration and workflow optimisation readiness.
- Look into governance: data privacy, security, vendor support, regulatory compliance (e.g., local health authority, FDA/CE). Check for adherence to standards like those from the American College of Radiology (ACR) or the Society of Radiographers (SoR).
6.2 Implementation tips: workflows, staff training, infrastructure
- Form a multidisciplinary team including radiologists, IT, data scientists, and clinical leadership. This supports human‑machine collaboration in diagnostics.
- Map current workflows: from scan acquisition (MRI/CT) → image reconstruction → reading/reporting. Identify where AI can help (e.g., segmentation‑classification pipeline MRI ML, triage of medical images using ML).
- Start with a pilot: choose a use case with clear benefit (e.g., improving turnaround time for brain MRI, or reducing radiation dose in CT).
- Train staff: radiologists should understand how the AI tool works (including explainable AI in medical imaging), how to interpret outputs, and when human oversight is needed.
- Ensure infrastructure readiness: high‑quality image data, integration with PACS/DICOM, adequate computing (edge or cloud), data security and privacy safeguards (for privacy‑preserving AI imaging).
- Set up monitoring and feedback: track performance over time, detect model drift, monitor false positives/negatives, and allow radiologists to give feedback to improve models.
6.3 Monitoring & auditing: performance tracking, model drift, update management
- Define key performance indicators (KPIs): e.g., reduction in reading time, change in diagnostic accuracy, reduction in radiation dose or contrast use (see AI for image quality & patient safety in CT and MRI).
- Use data audit trails: log AI decisions, radiologist overrides, error rates.
- Schedule periodic re‑validation: as new scanner models or protocols come in, the AI model may need re‑training or fine‑tuning.
- Set governance: define who is responsible for AI operations, updates, performance review, and compliance with regulations (see ACR’s ARCH‑AI programme).
6.4 Ethical & governance considerations: consent, data security, human‑in‑loop
- Inform patients when AI is used in their diagnostic imaging process.
- Maintain human oversight: AI should assist, not replace, the radiologist. Be cautious of over‑reliance risk.
- Ensure fairness: check for bias in AI medical imaging, ensuring the tool performs well across varied populations.
- Manage privacy: follow data protection regulations, anonymise imaging data when required, especially in workflows using federated learning MRI datasets or multi‑site data sharing.
- Clarify liability: who is accountable if AI output contributes to a wrong diagnosis? Have policies in place for decision‑making and auditing.
Conclusion
In summary, Artificial Intelligence (AI), Machine Learning (ML), and Deep Learning (DL) are changing how we use Magnetic Resonance Imaging (MRI) and Computed Tomography (CT) for diagnosis. These technologies help with image acquisition & reconstruction, image‑analysis: segmentation, detection, classification, and workflow optimisation & radiologist assistance. They support powerful tasks like brain tumour segmentation AI‑MRI, lung CT AI screening, and stroke detection with CT AI.
There are many benefits: improved diagnostic accuracy, faster scan times, reduced radiation dose, efficient radiology workflows, and personalised medicine via imaging AI. However, we must also recognise the challenges: issues of generalisation, explainable AI in medical imaging, bias in AI medical imaging, dataset heterogeneity in imaging AI, and regulatory and ethical hurdles.
The future is bright with advances like multimodal imaging machine learning, federated learning using MRI datasets, edge computing in imaging AI, and full‑pipeline AI models from scan to report. For clinicians, researchers, and health systems, success will depend on thoughtful implementation, strong data strategy, rigorous validation, and keeping the focus firmly on improving patient outcomes and safety.